Yellow Fever near Soddo
We have bad news and good news…
The bad news: there has been an outbreak of Yellow Fever in our region of Ethiopia, affecting about 35 people and killing 10.
The good news: Three of Soddo Christian Hospital’s staff members were instrumental in identifying the disease and reporting the outbreak to the World Health Organization, leading to the shipment of 1.5 million doses of the vaccine to Ethiopia.
 The discovery of the outbreak began when a patient showed up at our hospital with all the classic symptoms of Yellow Fever. But since that virus has not been present here in recent history, clinicians were hesitant to identify it as such right away. However, the next day another patient presented with similar symptoms and died. Then other patients at the hospital began telling our staff stories about people dying in a certain town – three of them in the same family!
The discovery of the outbreak began when a patient showed up at our hospital with all the classic symptoms of Yellow Fever. But since that virus has not been present here in recent history, clinicians were hesitant to identify it as such right away. However, the next day another patient presented with similar symptoms and died. Then other patients at the hospital began telling our staff stories about people dying in a certain town – three of them in the same family!
That’s when Dr. Ribka, Dr. Sok, and Nurse Woynishet reported their suspicions to the Zonal Health Officer, even though it was late on a Saturday night. Immediately, the CDC, WHO and UNICEF got involved with investigating, documenting and testing. Yellow Fever was indeed the confirmed diagnosis.
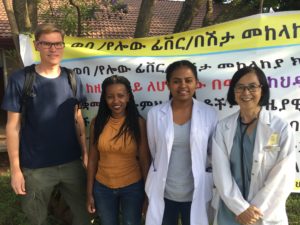
Photo L to R, Dr. Joakim, missionary infectious disease specialist from Sweden; Nurse Woynishet, works in ER and is responsible for reporting infectious diseases to health officials; Dr. Ribka, general practitioner; Dr. Sok, missionary internal medicine specialist.
 Thanks to the astuteness and persistence of our staff, 1.5 million Yellow Fever vaccines are now in Ethiopia. Our hospital is one of the immunization sites, having already immunized nearly 1,000 people since last Friday.
Thanks to the astuteness and persistence of our staff, 1.5 million Yellow Fever vaccines are now in Ethiopia. Our hospital is one of the immunization sites, having already immunized nearly 1,000 people since last Friday.
We are so very proud of our staff for acting quickly, containing the outbreak, and saving many lives!
Dr. Sok updating the SCH medical staff about the Yellow Fever outbreak and the containment strategy
The official news story at: https://in.reuters.com/article/us-ethiopia-yellowfever/yellow-fever-kills-10-in-ethiopia-who-ships-1-45-million-vaccines-idINKCN1NA2K3
Just like being here, you can make a difference, Amy Hinrichs writes about a visit to a rural clinic
“Is there money in the benevolence fund?” Dr. Mary asked me as we headed out to the rural clinic site near Ajora Falls. “I’m concerned Temegtu isn’t healing. I want to run some labs on him and get an ultrasound. I also want to bring him home with me so I can supervise his nutrition and wound care.”But Temegtu didn’t show up at clinic on Thursday. Fortunately, we know where he lives, so on the way home from clinic we stopped  and called out for him.
and called out for him.
Temegtu, his mother, siblings and neighbors gathered around the car as Dr. Mary explained her proposition. “I’d like to take Temegtu to Soddo Christian Hospital. He will stay at my neighbor’s house, but I will feed him and make sure he continues to get the care he needs so his skin infection can heal. Do I have your permission?”
I’m telling you, people…the relief, the gratitude of that mom…it was a sight to behold. If your son had an infection seemingly taking over his head, neck and chest, and you were powerless against it, how desperate would you feel? As we pulled away with Temegtu in the car, his mother (Dad was out working in the fields) and neighbors blessed us and thanked us over and over until we rounded the bend.
Guess what, though? We DIDN’T have any money in the benevolence fund. Since I was right there and had the money to help, I told Mary that Kurt and I would happily cover all his hospital and non-hospital costs. This is not a story about us, though, because you would have done the same thing if you’d been here.
Which is why I'm relaying this story to you...you can do the very same thing without being here in Ethiopia. I encourage you to be a blessing to others by becoming a monthly donor to the benevolence fund of Soddo Christian Hospital.

Go to soddo.org or click the blue button below to become a one-time or recurring donor to “Fund a Patient.” It's like being here.
Your gift can help
 On a beautiful day in Soddo, as I was walking to the playground with my children, I ran into our missionary internist who told me of a young adult woman who had come to the hospital in respiratory failure due to Guillain-Barre Syndrome. Her respiratory muscles were too weak to take in enough air and she was suffocating. She was 34 weeks pregnant. The medical team had quickly placed her on a breathing machine and obtained permission from the family to do a Cesarean section to save the baby’s life. The baby was requiring a lot of support for breathing, but was stable and the mom was in recovery.
On a beautiful day in Soddo, as I was walking to the playground with my children, I ran into our missionary internist who told me of a young adult woman who had come to the hospital in respiratory failure due to Guillain-Barre Syndrome. Her respiratory muscles were too weak to take in enough air and she was suffocating. She was 34 weeks pregnant. The medical team had quickly placed her on a breathing machine and obtained permission from the family to do a Cesarean section to save the baby’s life. The baby was requiring a lot of support for breathing, but was stable and the mom was in recovery.
As a new mother of a nearly 3-month old baby, my heart quickened for this mother, her other children and her family. As the week went on, despite our best care, the mother died. Baby was slowly taking in formula each day, but after a few days, developed some blood in his stomach, likely from necrotizing enterocolitis. This is one of the feared complications of premature birth, and the risk rises when a baby receives formula instead of breast milk. The baby could not eat for a few days and started to get malnourished. There was no way for him to get breast milk from his mother, and the family had left to prepare for her burial. So who would pay for this child’s care? Unlike America, there is no medical insurance or Medicaid for orphans and widows. If a patient cannot pay for medical care in cash at the time of service, most places will turn the patient away. So this motherless child was left in our NICU without family and without much to eat for nearly 7 days. Thanks to some of our dedicated supporters, we had money in our benevolence fund to pay for this child’s hospitalization and we didn’t have to send him away.
As I sat at home and fed my own baby, I felt the grief of this child and his family and prayed for this baby. I felt that I needed to pump extra milk for this orphaned child, so I did.
Psalm 10:14 says, “But you, God, see the trouble of the afflicted. You consider their grief and take it in hand. The victims commit themselves to you; you are the helper of the fatherless.”
Our missionary community rallied around this child. I pumped for the baby, and we fed him through his nasogastric tube. As we started feeding him, he was comforted, cried less and tolerated his feeds. Our community of workers and NICU staff took turns holding baby throughout the day to give him attachment, love, prayers, and touch. The busy NICU staff commented that baby would be crying, but when someone came to hold him, he stopped.
We gave him everything we could: fluids, antibiotics, oxygen, a blood transfusion, physical touch, donated breast milk, and prayers. My heart was full of joy. He was flourishing, happy and felt a little like a part of our family. Then suddenly, he developed a fever and rash and died less than 18 hours later. I cried…a lot. As I walked home from the hospital, having just declared his death and completed the paperwork, God reminded me this boy was loved. He was placed into a family, our Soddo family. He was touched and held, and now he is with is mother. It was difficult to accept this as I walked home to my healthy 3 month old baby, but in this matter I have no choice.
It is a blessing to be a part of this hospital and this loving and caring team, even in difficult times. Yet now our benevolence fund is empty. We have to pay our staff a living wage and therefore cannot provide free care to everyone. So the dilemma exists: what do we do when faced with the poor, the widow, the orphan? Do we simply turn them away and not care for their medical needs? I am asking you to consider giving generously to our benevolence fund so we can be the light of Christ and the hands of God together as an international team that extends beyond the borders of our hospital grounds to those that come to our hospital’s door. Would you partner with us?
Our wonderful staff: Giving back however they can
 One of our recent visiting residents wrote about his week at Soddo Christian Hospital this summary of his visit:
One of our recent visiting residents wrote about his week at Soddo Christian Hospital this summary of his visit:
“We do what we can”
It takes a huge team to care for patients here. This picture is of the multidisciplinary team that makes orthopedic rounds each day. They do a wonderful job in very challenging situations. Our staff every day confront medical needs that challenge both their medical skills and their emotional fortitude. The orthopedic surgery resident from UCLA just finishing his week-long surgical rotation at Soddo summarizes his experience below.
“It’s been a tough week here. There are so many people that come to Soddo Christian Hospital from all over the eastern part of Africa and Ethiopia, and there are only so many resources and only so much time in a day to help people. There is such an inundation of trauma from road traffic accidents, and [so many] infections [because of] people waiting to see physicians or travelling for days to come to this hospital, that the operating room is reserved for the [most] serious of emergencies. Emergencies that would be deemed emergencies in the United States are true emergencies here, too, but the timing of treating them is delayed, with a certain amount of triage that [must occur]. For example, hip fractures are generally treated within 24-48 hours to reduce morbidity and complications from immobility and pain. [But] we’ve had a patient in the hospital who has had a hip fracture for 2 months, who arrived last week. He’s in need of hip implants, which are coming, but are waiting at customs in Addis Ababa. They should arrive next week.
“It’s hard to see patients in clinic who have real problems that are solvable with the right resources: osteoarthritis treated with knee or hip replacements, ACL or PCL injuries treated with arthroscopic reconstructions, or even basic fractures like tibias, femurs, forearms or elbows. Many are treated in a delayed fashion because of the need to take care of infections or open fractures. [See the two children pictured.] Many emergency patients sleep in the yard of the hospital waiting for a bed. It’s heart-wrenching to see children who can’t walk because of neglected, infected hips that have destroyed the joint, or complications from things like TB and polio, which are so rare in the US.
“Over the past week, we’ve had some complex cases. As a team, we were able to perform 2 complex pelvic operations; a scapula/glenoid fracture was fixed, as well as multiple open femur and tibia fractures, along with a few pediatric fractures due to traffic accidents. Additionally, we had a couple of patients with multiple knee ligament injuries. Given my interest in sports medicine, and the presence of an arthroscopy tower in the OR (one of the few in the country), Dr. Anderson challenged me to take care of a couple of the knee ligament injuries and expose the Ethiopian residents to arthroscopy. I quickly realized that arthroscopic surgery here would be extremely challenging: the language barrier, the power goes out frequently, [and] the staff is used to dealing with trauma [injuries so] all [the] arthroscopic instruments are new [to them]. Additionally, these injuries were difficult as multiple ligaments were injured, and we would be reconstructing multiple ligaments at a time. [Seeing my hesitation], Dr. Anderson motivated me by explaining that we were likely the only people in Ethiopia who had the equipment and the ability to treat these injuries.
 “[W]e ran 4 operating rooms at the same time. One Ethiopian resident took consults in the Emergency Room, one Ethiopian resident operated on infections and long bone fractures, Dr. Anderson and another Ethiopian resident fixed a complex pelvic fracture, and the fourth Ethiopian resident helped me with [the] arthroscopic PCL reconstruction and used the fluoroscope machine to fix a complex tibia fracture. We all made it through. And when we were done, the knee felt stable, the pelvis was fixed, and 8 other infected bones and fractures were clean and fixed. It was a tough, long day, but in retrospect, we accomplished a lot as a team.
“[W]e ran 4 operating rooms at the same time. One Ethiopian resident took consults in the Emergency Room, one Ethiopian resident operated on infections and long bone fractures, Dr. Anderson and another Ethiopian resident fixed a complex pelvic fracture, and the fourth Ethiopian resident helped me with [the] arthroscopic PCL reconstruction and used the fluoroscope machine to fix a complex tibia fracture. We all made it through. And when we were done, the knee felt stable, the pelvis was fixed, and 8 other infected bones and fractures were clean and fixed. It was a tough, long day, but in retrospect, we accomplished a lot as a team.
“As I reflect on my last day operating here, I think there’s a bright outlook for this country. I’m encouraged that I helped expose the Ethiopian residents to arthroscopic surgery. I feel grateful to see that [my supervising doctors] have trained me to perform these cases independently. Lastly, I was very impressed with the Ethiopian residents. They are smart and extremely well read. Dr. Anderson’s knowledge and ability is impressive. Soddo Christian Hospital’s resources, though limited compared to the USA, provide an orthopedic mecca for the Ethiopian residents here. I’m hopeful that the partnership with UCLA/OIC can continue to bring US residents with different interests to Ethiopia where we can learn from Dr. Anderson and the residents—and give back however we can.”
Another Miracle
Dr Michelle Yates writes:
"Sometimes we have those days or experiences that drastically change the way we think of life. Sometimes I’m aware enough to realize it, and other days I’m too dense to see what is right in front of me. An encounter with a special family has rocked my faith and my medical world view.
This story has two unique parts, the medical amazement and the personal story. As a human being we cannot disconnect the two, but let me tell it as it was revealed to me.
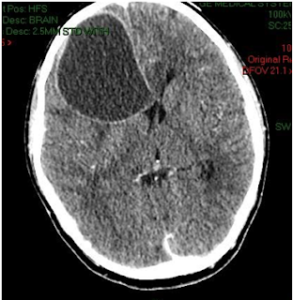
A 12-year-old boy from a rural area of Ethiopia (12-15 hours transport to get to Soddo) arrives nearly comatose, unable to sit, unable to move his entire right side, unable to eat, barely able to speak. He had a fever and a rigid neck. He had signs of increased pressure in his brain. I couldn’t do a lumbar puncture to confirm my suspicion of meningitis and our CT scanner, the only within 3 hour drive, was not working. He had already been on IV antibiotics for 2 weeks and didn’t get any better. His father, in desperation, brought him to our hospital traveling 2 days on a bus. I changed his antibiotics, gave him some steroids, waited for our CT scanner to be fixed and prayed. I treated him for a possible brain abscess, a complication of meningitis, but knew the entire time it could all be from aggressive cancer. Problems with import paperwork kept our CT scanner down for another 10 days.
He got a little better with medications, but I still wasn’t sure exactly what I was treating. When I finally got the CT scan of his head, we saw the very large brain abscess. It was the biggest I had ever seen. I tried to convince the dad to go see the neurosurgeon many hours away, but he said he could not, he had used all the money he had to get him to our hospital. So I discussed the case with our general surgery team, and they thought they could try to place a drain into the brain through a hole drilled in the skull to remove the infection and give the medicine a chance to work. By the grace of God, the procedure was a success and with no complication the infectious abscess was all drained! What a miracle. We continued his IV antibiotics for another 6 weeks and all his symptoms were gone, except a little bit of scarring in his eye. It was such a blessing to be a part of his recovery. The family is very poor and his hospital care was paid for by our benevolence fund supplied by generous donations. Without this financial support, this boy would have died.
But this is only half the story. I heard little bits here and there throughout his hospital stay, but the day before discharge we gathered to give this boy a going away party with Coke and popcorn and cookies. Our staff needs to celebrate the wins in our department. As in any good Ethiopian party, there were lots of speeches. The dad thanked our pediatric team for our care and went on to tell his story from his perspective.
He tells us that his son is the light of his life. 12 years ago, when he was 1 month old, his mother died suddenly and tragically. This single event earned this boy the title gefee, “the child that pushed his mother out” or more bluntly, “the mother killer”. In his culture, these children are often hated by the family, and sometimes in certain areas killed and buried with their mother. Despite this title of hatred given him at only 1 month of age, his father loved him. Because of his love for his son, this father was outcast from his family and his town. He had just lost his wife, and now had lost his community. He had to live on the edge of town and scrape by to get him enough food for him and his infant son because formula milk and cow’s milk is very expensive. The dad told us that this young boy barely left his side for years because others around him would give him a difficult time. Against cultural stigma and grief, this dad loved and protected his child.
In the middle of his speech, this father falls to his knees and cries out asking God for forgiveness, forgiveness for his unbelief. He tells us that after a few days in the hospital, he went to our hospital bathrooms and wept. He has no money. His treasured son is so sick. He has lost everything to have this boy, and now he has used the last of his savings for nothing. He will have to carry home a dead body. He was asking God where he would get the money to pay for the transport of the dead body home. He tells us that God called back to him and told him to stand up and to come to his throne of grace, undeserved grace. He tells us that it was that day (7 weeks before) we placed his son on our benevolence fund and now his son is walking home. He cried out again to thank God for his mercy and grace and asked once again for forgiveness for his lack of faith that God could heal his son and give him all the money he needed.
As I listened to his story, I was simply struck by the extreme hardship faced by this young boy and his family. I was so thankful that we could love him well at our hospital. Simply put, This is why we are here. I was also convicted. How often do I ask God for miraculous healing of my patients, myself, my friends or family? Do I repent when I lack faith for his healing touch? How often do I forget to trust God to cover all my financial needs? Do I cry out to Him when I feel I am at the end of my capacity? Do I truly believe that he will give everything he promises?
Because of this father and son I am forever changed.
Amazing transformation

A young man came to our hospital from a region to the east. Something was causing pain in his leg, so he and his best friend traveled to Soddo Christian Hospital because they knew he would receive excellent care.
About a year ago, a group of Ethiopian Christians from Soddo went to the region of these young men to share the gospel. However, the outreach group purposely decided not to go to the village of these two men because of the violent reputation of this tribe. They are known for killing up to 30 people in retribution for a single offense.
While the patient and his friend, both from this violent tribe, were at Soddo Christian Hospital, they watched the Jesus Film, and one of our hospital chaplains visited with them. God had touched the heart of the patient's friend, and he was gloriously saved! Not only that, but the new believer is the son of the king of this tribe. He has returned to his home, eager to share the love and truth he found in Christ with his family and tribe.
The son of a king has become a son of the King of Kings. There is much rejoicing here.
Surgical Treatment of Chronic Elbow Dislocation Allowing for Early Range of Motion: Operative Technique and Clinical Results
Surgical Treatment of Chronic Elbow Dislocation Allowing for Early Range of Motion: Operative Technique and Clinical Results
This is the largest case series of surgically treated patients with chronic elbow dislocation. Using our surgical technique, 97% of patients had good or excellent outcome with a low complication rate. Open reduction of chronic elbow dislocation can be accomplished while permitting early motion with minimal recurrent dislocation risk.
We have developed a straightforward surgical technique that allows for early elbow range of motion (ROM) with a little risk of recurrent instability. We present the operative technique and results of this surgical technique from 2 tertiary centers in Ethiopia. Our hypothesis is that our surgical technique and postoperative rehabilitation protocol allows for good patient outcome regardless of injury duration.
Duane R. Anderson, MD,* Justin M. Haller, MD,† Lucas A. Anderson, MD,† Samuel Hailu, MD,‡ Abebe Chala, PT,* and Shawn W. O’Driscoll, MD, PhD§
Our Pediatric ward is crowded

 This week, I was amazed at how crowded the hospital grounds are. I quickly learned that families stay on the property when their loved ones are hospitalized. When all beds are filled, which is a common occurrence, some sick and injured patients stay in the yard waiting for a vacancy. Families huddle together, sleep under a tree or under the shelter of overhangs with few complaints. Above, is the pediatric ward, which is one large room with multiple beds. It is not uncommon to see family members share a bed or sleep on the ground next to the hospital bed. For those who have not been here, imagine 6 hospital beds and 6 families, sharing one large room.
This week, I was amazed at how crowded the hospital grounds are. I quickly learned that families stay on the property when their loved ones are hospitalized. When all beds are filled, which is a common occurrence, some sick and injured patients stay in the yard waiting for a vacancy. Families huddle together, sleep under a tree or under the shelter of overhangs with few complaints. Above, is the pediatric ward, which is one large room with multiple beds. It is not uncommon to see family members share a bed or sleep on the ground next to the hospital bed. For those who have not been here, imagine 6 hospital beds and 6 families, sharing one large room.
Today, we took care of a 4 year old child who had fallen from a mango tree, had an open distal radius and ulna fracture with the radius coming out of the skin. There was mud and grass on the visible end of the bone coming through the skin. We were able to take the patient to the operating room, remove the debris and mud, reduce the fracture and pin it back into place. Dilute bleach is used as irrigation in the operating room, and almost every patient’s wounds are cleaned with dilute bleach daily while they are in the hospital. It has proven to be extremely effective.
I am grateful to UCLA and OIC to have had the opportunity to come visit and help in Ethiopia, and look forward to another exciting week!
Would you consider a gift to our Benevolence Fund to help our poorest patients?
These notes and photos were provided by:
> Ed Cheung
> UCLA Orthopaedic Surgery
Yehone, "his name means, "Let it be"

![]()
![]()
 Yehone is a newborn baby at Soddo Christian Hospital. “Let It Be” is the meaning of his name, but that is an impossible task for his young mother and grandmother, both of whom anxiously await the outcome of a surgery on which they’ve just been debriefed. Yehone’s family has traveled to Soddo from their local hospital 50 kilometers away. His grandmother explains that Yehone is the first-born child of her daughter, who is young, fatherless, and recently married. The tiny child in her arms is the prize of this family. Twenty days after his birth, Yehone’s family knew that he was fatally ill, with a distended stomach and unrelenting vomiting. They sought diagnoses and treatment at the hospital nearest them, but did not have enough money to pay for the child’s care. They were sent to Soddo Christian Hospital, where a Benevolence Fund will help pay for life-saving treatment they cannot afford. Yehone’s family used everything they had to make it to the hospital in Soddo. Today, Yehone will undergo an operation to heal the root of his illness - an intestinal malrotation.
Yehone is a newborn baby at Soddo Christian Hospital. “Let It Be” is the meaning of his name, but that is an impossible task for his young mother and grandmother, both of whom anxiously await the outcome of a surgery on which they’ve just been debriefed. Yehone’s family has traveled to Soddo from their local hospital 50 kilometers away. His grandmother explains that Yehone is the first-born child of her daughter, who is young, fatherless, and recently married. The tiny child in her arms is the prize of this family. Twenty days after his birth, Yehone’s family knew that he was fatally ill, with a distended stomach and unrelenting vomiting. They sought diagnoses and treatment at the hospital nearest them, but did not have enough money to pay for the child’s care. They were sent to Soddo Christian Hospital, where a Benevolence Fund will help pay for life-saving treatment they cannot afford. Yehone’s family used everything they had to make it to the hospital in Soddo. Today, Yehone will undergo an operation to heal the root of his illness - an intestinal malrotation.
Dr. Michelle explains to the mother and grandmother the need for this operation, assuring them that God has already protected their child, that his life today is reason to give thanks to God, and that we must continue to entrust the child’s care to God through prayer. Ayellech, a hospital chaplain, is in the room to pray for the baby and family. The women are both timid, they are afraid of the surgery and do not believe their precious one will make it through; “He is so small,” what if he does not wake up? The gnawing, clenching feeling of fear is evident on the women’s faces. Ayellech places her hands on the child and his mother, and prays powerfully for the baby’s life. When the prayer finishes, she does not stand up and walk away. She holds the mother’s shoulder and asks, “Why did you not say ‘Amen?’” Do you not know that God is good? The women look worried, but they know that this is their hope, that they must put their trust in the doctors here to save their child; it is through the faith and evangelism of the staff that they are led instead to  put their faith in God. “God is the only physician who can save this baby,” Dr. Yates explains before she prays for the family, “So we must pray.”
put their faith in God. “God is the only physician who can save this baby,” Dr. Yates explains before she prays for the family, “So we must pray.”
“God has given us an opportunity to share the gospel here…to people who come from all corners and all tribes of Ethiopia,” explains Tesfaye, another hospital chaplain, “I cannot share the gospel more anywhere else.”
Soddo Christian Hospital provides more than physical healing, but it is only through the lifesaving care of the doctors that this opportunity arises.
When Yehone’s family arrived at Soddo, they had spent everything they had on transportation to the hospital. They had nothing left to pay for treatment.
The Benevolence Fund is currently very short of funds. We used $113,000 to fund Benevolence Patients in 2016, wiping out our reserves.
 For Yehone and his family, the hospital’s reserve Benevolence Fund (which has been set aside for pregnant mothers) is being re-allocated to cover the surgery and medicine costs for Yehone, in addition to food for his mother and grandmother. Because of this resource, Yehone and his family will remain in the hospital while he undergoes treatment; they will be in the care of the hospital’s doctors, nurses, and chaplains, who will continue to share with them the love of Christ, and the hope of new life given by Jesus.
For Yehone and his family, the hospital’s reserve Benevolence Fund (which has been set aside for pregnant mothers) is being re-allocated to cover the surgery and medicine costs for Yehone, in addition to food for his mother and grandmother. Because of this resource, Yehone and his family will remain in the hospital while he undergoes treatment; they will be in the care of the hospital’s doctors, nurses, and chaplains, who will continue to share with them the love of Christ, and the hope of new life given by Jesus.
There is now an immense need to replenish the hospital’s Benevolence Fund, which in the past has been lifesaving to hundreds of patients – thanks to the generosity of donors. This is a major resource to provide opportunities for the staff to serve the poor; it is the means through which Soddo Christian Hospital shares the gospel with those who both need and desire it the most.
With your donation, Soddo Christian Hospital can continue to provide this much-needed care and hope to the neediest in Ethiopia. Will you help?
Yehone’s surgery was successful. He is now recovering! Thank you God!
You can give online at:




